There is a disease that creeps upon us after age 50, especially in women. This is a bone disease known as Osteoporosis. For those looking for answers regarding this disease, this article should shed some light as it explores Osteoporosis: The Facts.
What is Osteoporosis?
Osteoporosis is a bone disease. It is a condition that causes bones to become weak and brittle. This can eventually lead to bone fractures from a fall or, in serious cases, from sneezing or minor bumps. Osteoporosis means “porous bone.”
What is Osteoporosis Caused By?
Osteoporosis occurs when the body doesn’t make enough bone, loses excessive amounts of bone, or both. Our bones are in a perpetual state of renewal — new bone is produced and old bone is discarded. In our youth, the body produces new bone faster than it tears down old bone, and the bone mass increases. After the early 20s, this process slows down, and a majority of individuals reach their maximum bone mass by age 30. As individuals age, bone mass is diminished faster than it is produced.
How viable we are to develop osteoporosis depends somewhat on what amount of bone mass we accumulate in our youth. Peak bone mass is to some extent inherited and varies additionally by ethnic group. The higher our peak bone mass, the more bone we will have in reserve, the less likely we are to develop osteoporosis as we age.
Risk Contributors
Several markers can increase the likelihood that an individual can develop osteoporosis — including race, age, lifestyle choices, and underlying medical conditions and treatments.
Some of these are out of our control, these include:
- Race. There is the greatest risk of osteoporosis if an individual is white or of Asian descent.
- Sex. Women are considerably more prone to develop osteoporosis than men are.
- Age. The older an individual gets, the greater the risk of developing osteoporosis.
- Body frame size.
Individuals, both men, and women who have small body frames are likely to have a higher risk because they may have less bone mass to draw upon as they age. - Family history.
Having a parent or sibling with osteoporosis puts one at greater risk, especially if their mother or father fractured a hip.
Other risk contributors some of which we can control include:
Hormone Levels – Osteoporosis is most likely to occur in people who have an excess or deficiency of certain hormones in their bodies. Examples are:
- Thyroid problems.
Excessive amounts of thyroid hormone can cause bone loss. This can occur if the thyroid is overactive or if an individual takes a disproportionate amount of thyroid hormone medication to treat an underactive thyroid. - Sex hormones.
Decreased levels of sex hormones tend to weaken bone. The reduction of estrogen levels in females during menopause is one of the greatest risk factors for developing osteoporosis.
Men, as they age, have a gradual reduction in testosterone levels. Treatments for prostate cancer that diminish testosterone levels in men and treatments for breast cancer that diminish estrogen levels in women are likely to hasten bone loss.
- Additional glands.
Osteoporosis has additionally been linked with overactive parathyroid and adrenal glands.
Diet – Osteoporosis is in all probability to occur in individuals who have:
- Low calcium intake.
A lifelong deficiency of calcium plays a part in the advancement of osteoporosis. Low calcium intake contributes to weakened bone density, premature bone loss, and a heightened risk of fractures. - Eating disorders.
Strictly restricting food intake and being underweight diminishes bone in both men and women. - Gastrointestinal surgery.
Surgery to reduce the size of the stomach or to remove part of the intestine restricts the amount of surface area accessible to absorb nutrients, which includes calcium. These surgeries include those to help an individual lose weight and for other gastrointestinal issues.
Medications – Long-term use of corticosteroid medications either oral or injected, such as prednisone and cortisone, impedes the bone-rebuilding process. Osteoporosis has also been linked with medications used to fight or prevent such conditions as:
- Gastric reflux
- Seizures
- Transplant rejection
- Cancer
Underlying Medical conditions
The probability of osteoporosis is higher in individuals who have specific medical conditions, including:
- Cancer
- Celiac disease
- Inflammatory bowel disease
- Kidney or liver disease
- Lupus
- Multiple myeloma
- Rheumatoid arthritis
Lifestyle choices – Some lifestyle habits can increase the risk of osteoporosis. These include:
- Inactive (Sedentary) lifestyle. Individuals who spend a lot of time sitting have an elevated risk of osteoporosis than do those that are more active. Any weight-bearing exercise and activities that advance balance and good posture are beneficial for the bones, but in particular, walking, running, jumping, dancing, and weightlifting seem especially helpful.
- Excessive alcohol intake. Regular intake of more than two (2) alcoholic drinks a day increases the risk of osteoporosis.
- Tobacco usage.
The specific part tobacco plays in osteoporosis is not apparent, however, it has been shown that tobacco use contributes to weakened bones.
What are the Symptoms of Osteoporosis?
There usually are no symptoms in the early phase of bone loss. However, once the bones have been weakened by osteoporosis, an individual might have warnings and symptoms that include:
- A stooped posture
- Back pain, produced by a cracked or collapsed vertebra
- Loss of height over time
- A bone that fractures a great deal more easily than expected
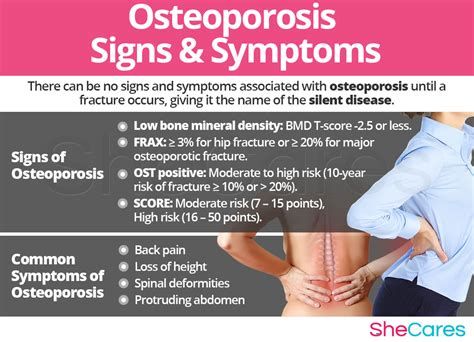
Even without symptoms, an individual may want to consult with a doctor about osteoporosis if they have gone through early menopause or took corticosteroids.
What are the complications of Osteoporosis?
Bone fractures are the most serious complications of osteoporosis, particularly in the spine or hip. Hip fractures are frequently caused by a fall and can subsequently result in disability and even an amplified risk of death within the first year after the injury.
In some cases, spinal fractures can happen even without a fall. The bones that make up the spine (vertebrae) can weaken to the point of crumbling, which can result in back pain, shortened height, and a bent forward posture.
Treating Osteoporosis
Diagnosis
The first step in diagnosing osteoporosis is to test the density of the bones. Bone density is measured by a machine that makes the use of low levels of X-rays to establish the proportion of mineral in the bones. During this 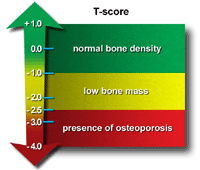 painless test, the patient lies on a padded table as a scanner passes over the body. In a majority of cases, only a few bones are checked — generally the hip and spine. A score of -2.0 or lower indicates an osteoporosis condition.
painless test, the patient lies on a padded table as a scanner passes over the body. In a majority of cases, only a few bones are checked — generally the hip and spine. A score of -2.0 or lower indicates an osteoporosis condition.
Treatment
Treatment recommendations are usually based on an estimate of the risk of breaking a bone in the next ten years using information such as the results of the bone density test. If the risk is not high, treatment may not include medication and instead might focus on modifying risk factors for bone loss and falls.
For both males and females at increased risk of fracture, the most widely prescribed osteoporosis medications are called bisphosphonates. Some common names include:
- Alendronate (Binosto, Fosamax)
- Ibandronate (Boniva)
- Risedronate (Actonel, Atelvia)
- Zoledronic acid (Reclast, Zometa)
You may recognize some of these names from television commercials.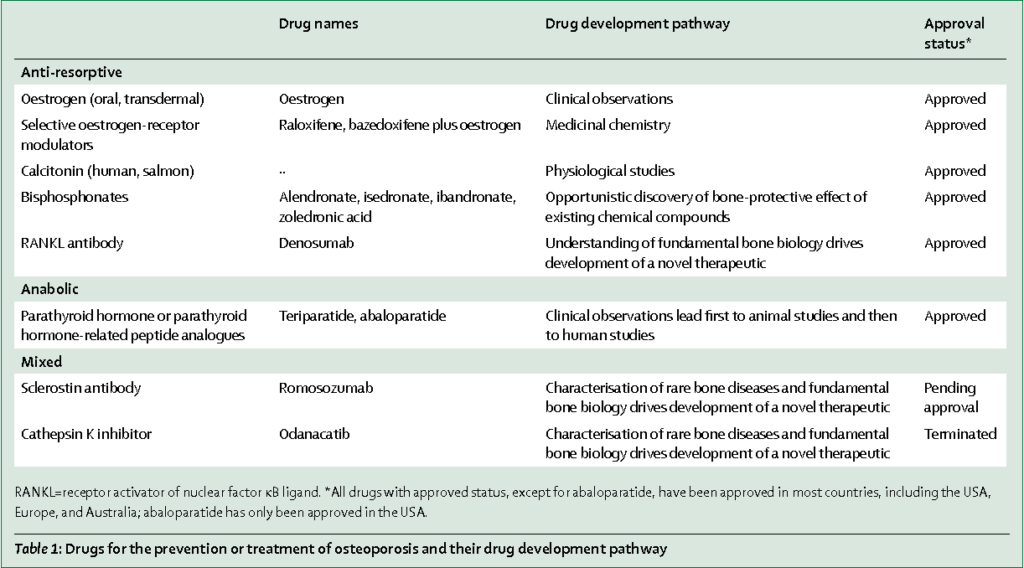
Side effects can include abdominal pain, nausea, and heartburn-like symptoms. These are less probable to occur if the medication is taken correctly.
There are intravenous forms of bisphosphonates that do not cause stomach upset but can cause headache, fever, and muscle aches for up to three (3) days. It may be easier to schedule a quarterly or yearly injection than to recall taking a weekly or monthly pill; however, it can be more expensive to do so.
Another class of drugs is Monoclonal antibody medications.
In comparison with bisphosphonates, denosumab (Prolia, Xgeva) generates comparable or better bone density results and decreases the chance of all types of fractures. Denosumab is delivered via an injection under the skin every six (6) months.
If denosumab is chosen, the patient may have to continue to do so for an indefinite period. Recent research denotes that there could be a high risk of spinal column fractures after terminating the drug.
A very rare complication leading to a combination of bisphosphonates and denosumab is a break or crack in the middle of the thighbone.
A second rare difficulty is delayed healing of the jawbone (osteonecrosis of the jaw). This can come about after an invasive dental procedure such as a tooth extraction.
Patients should have a dental examination before commencing these medications, and continue to take good care of their teeth and see the dentist regularly while on them. Therefore, they must make sure their dentist knows that they are taking these medications.
Another form of treatment is hormone-related therapy
Estrogen, especially when started shortly after menopause, can assist in maintaining bone density. On the other hand, estrogen therapy can heighten the risk of endometrial cancer, breast cancer, blood clots, and possibly heart disease. Consequently, estrogen is normally used for bone health in younger women or in women, whose menopausal symptoms also need treatment.
Raloxifene (Evista) imitates estrogen’s favorable effects on bone density in postmenopausal women, without some of the risks connected with estrogen. Engaging this drug can reduce the risk of some types of breast cancer. Hot flashes are a common side effect. Raloxifene additionally may increase the risk of blood clots.
In men, osteoporosis might be coupled with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help in lessening the symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and therefore are recommended by them or in addition to testosterone.
Lastly, there are bone-building medications.
If an individual cannot tolerate these more common treatments for osteoporosis — or if they do not work well enough, a health-care practitioner might suggest trying one of these:
- Teriparatide (Forteo).
This powerful drug is comparable to parathyroid hormone and stimulates new bone growth. It is administered by daily injection under the skin. After two (2) years of treatment, another osteoporosis drug is used to maintain the new bone growth. - Abaloparatide (Tymlos) is an additional drug comparable to parathyroid hormone. It can only be taken for only two (2) years, which will be followed by another osteoporosis medication.
- Romosozumab (Evenity).
This is the most recent bone-building medication to treat osteoporosis. It is administered by injection every month at a physician’s office. It is limited to one (1) year of treatment, followed by other osteoporosis medications.
How to Prevent Osteoporosis
Proper nutrition and regular exercise are vital for keeping bones healthy throughout life.
Protein
Protein is one of the structure blocks of bone. However, there is conflicting evidence regarding the impact of protein intake on bone density.
Most people get ample amounts of protein in their diets, however, some do not. Vegetarians and vegans can get ample protein in the diet if they purposely seek suitable sources, such as nuts, soy, legumes, and seeds for vegans, vegetarians, and eggs and dairy for vegetarians.
Older adults may eat less protein for a variety of reasons. If you think you are not getting enough protein, ask your doctor if supplementation is an option. For more information on protein, you may read the article, The Facts about Proteins,
on this website.
Weight
Being underweight multiplies the chance of bone loss and fractures. Additional weight is now known to increase the risk of fractures in the arm 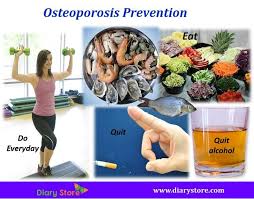 and wrist. As such, maintaining appropriate body weight is good for bones just as it is for health in general.
and wrist. As such, maintaining appropriate body weight is good for bones just as it is for health in general.
Calcium
Both males and females between the ages of 18 and 50 require 1,000 milligrams of calcium a day. This daily amount rises to 1,200 milligrams when women turn 50 and men turn 70.
Excellent sources of calcium include:
- Calcium-fortified cereals and orange juice
- Canned salmon or sardines with bones
- Dark green leafy vegetables
- Low-fat dairy products
- Soy products, such as tofu
If an individual finds it difficult to get enough calcium from their diet, they should consider taking calcium supplements. However, they must keep in mind that too much calcium has been linked to kidney stones. Although yet uncertain, some experts propose that too much calcium especially in supplements can increase the risk of heart disease.
The Health and Medicine Division of the National Academies of Sciences, Engineering and Medicine (formerly the Institute of Medicine) recommends that the sum of calcium intake, from supplements and diet, combined, should be no more than 2,000 milligrams daily for individuals older than 50.
Vitamin D
Vitamin D improves the body’s ability to take in calcium and improve bone health in other ways. Individuals can get some of their vitamin D from sunlight, but this may well not be a good source if people who live in high latitude, if they are housebound, or if they regularly use sunscreen or avoid the sun because of the risk of skin cancer.
To get enough vitamin D to maintain bone health, it is recommended that adults between the ages 51 to 70 get 600 international units (IU) and 800 IU a day beyond age 70 by way of food or supplements.
Individuals without other sources of vitamin D and especially those with limited sun exposure might need a supplement. Most multivitamin products contain between 600 and 800 IU of vitamin D. Up to 4,000 IU of vitamin D a day is safe for most people.
Vitamin K2
Vitamin K2 plays a key role in the metabolism of calcium, which the primary mineral found in our bones and teeth. It triggers the calcium-binding actions of two (2) proteins — matrix GLA protein and osteocalcin, which aid in building and maintaining bones.
There is additionally substantial evidence from controlled studies that K2 may provide major benefits for bone health.
Vitamin K2 is produced by gut bacteria in the large intestine. There is some evidence that suggests that broad-spectrum antibiotics contribute to a K2 deficiency. However, the average intake of this important nutrient is incredibly low in the modern diet.
Vitamin K2 is principally found in specific animal and fermented foods, in which most individuals do not consume a large amount. Abundant animal supplies include high-fat dairy products from egg yolks, grass-fed cows, as well as liver and other organ meats. Vitamin K is fat-soluble, meaning low fat and lean animal products do not contain an abundance of it.
Animal foods have the MK-4 subtype, while fermented foods such as sauerkraut, natto and, miso pack more of the longer subtypes, MK-5 to MK-14.
If these foods are inaccessible, taking supplements is a valid alternative. The benefits of supplementing with K2 may be improved even further when combined with a vitamin D supplement since these two vitamins have synergistic effects. An excellent selection of vitamin D and K2 supplements can be found at THE VITAMIN SHOPPE.
Exercise
Exercise can assist in building strong bones and slow bone loss. It is never too late to start, but the most benefit will be gained if regular exercise is started during one’s youth and continues throughout life.
It is advisable to combine strength-training exercises with weight-bearing and balance exercises. Strength training aids in strengthening muscles and bones in the arms and upper spine. Weight-bearing exercises such as jogging, stair climbing, walking, running, skipping rope, skiing, and impact-producing sports — affect mainly the bones in your legs, hips and, lower spine. Balance exercises such as tai chi can reduce the risk of falling especially as one gets older.
Swimming, cycling, and exercising on machines such as elliptical trainers can yield a good cardiovascular workout, but they do not improve bone health.
Please leave any questions, comments, and concerns below.
Good Health!!
Great input Nathaniel,
My friend has been having problems with his limbs and it’s been around for a month now and when he’s reluctant to go to the clinic to check but I have a feeling he might have osteoporosis as he lacks calcium, do you think it might really be osteoporosis? If so, then I really need to get him so supplements to help him out.
Well it is possible Riaz but he should get himself checked out very soon. If he does have osteoporosis he will need more than supplements.