The death of Chad Bosman, the actor, has raised awareness and concern for 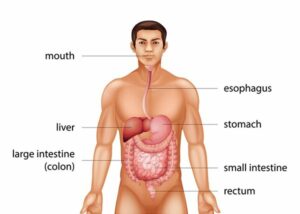 colon cancer. The purpose of this article is to inform readers about the facts on colon cancer.
colon cancer. The purpose of this article is to inform readers about the facts on colon cancer.
What is Colon Cancer?
Cancer is abnormal cell growth. Colon cancer is cancer that starts in the colon, also known as the large intestine. The colon is the closing stretch of the digestive tract.
Colon cancer is occasionally called colorectal cancer, which is a term that links colon cancer and rectal cancer, which commences in the rectum.
Causes of Colon Cancer
Colon cancer typically starts as small, benign (noncancerous) masses of cells called polyps that develop on the inside of the colon. Over time, a few of these polyps can become cancerous, forming colon cancers. Colon cancer usually affects older adults, although it can happen at any age.
Actually, physicians are not sure what the cause of most colon cancers is.
Generally speaking, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. Within a cell’s DNA is a set of instructions that instruct it on what it should do.
Healthy cells grow and divide in an orderly and systematic way to keep the body functioning normally. However, when a cell’s DNA is flawed and becomes cancerous, cells continue to divide — even when new cells aren’t needed. As the cells accumulate, they form a tumor.
Over time, the cancer cells can increase to invade and destroy normal nearby tissue. Also, these cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Risk Factors
There are some factors that can increase the risk of developing colon cancer which include:
- Age. Colon cancer can be detected at any age, but a more significant number of people with colon cancer are older than 50. The rates of colon cancer in people younger than 50 have been on the rise, but doctors are not sure why.
- Race. African-Americans have an increased risk of colon cancer individuals of other races.
- Personal history. If an individual has already had colon cancer or noncancerous colon polyps, there is a greater risk of colon cancer in the future.
- Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn’s disease, can add to the risk of colon cancer.
- Inherited syndromes. Some gene mutations passed through generations of a family can increase the risk of colon cancer considerably. It is only a small percentage of colon cancers linked to inherited genes.
- Family history. An individual is more likely to develop colon cancer if he or she has a blood relative who has had the disease. If more than one family member has or previously had colon cancer or rectal cancer, the risk is even greater.
- Diet. Low-fiber, high-fat. Colon cancer and rectal cancer links with a typical Western diet, which is low in fiber and high in fat and calories. Research conducted in this area has had mixed results. Some studies have found an increased risk of colon cancer in individuals who consume large amounts of red meat and processed meat.
- A sedentary lifestyle. Inactive individuals are more likely to contract colon cancer. Getting regular physical exercise may reduce the risk of colon cancer.
- Diabetes. Individuals with diabetes or insulin resistance have a heightened risk of colon cancer.
- Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered average weight.
- Smoking. People who smoke may have a heightened risk of colon cancer.
- Alcohol. Heavy consumption of alcohol amplifies the risk of colon cancer.
- Radiation therapy. Radiation therapy for cancers directed at the abdomen to treat previous cancers increases the risk of colon cancer.
Symptoms of Colon Cancer
Most individuals with colon cancer do not experience any symptoms in the early stages of the disease. When symptoms appear, they tend to vary,  depending on the size of the cancerous cells and the location in the large intestine.
depending on the size of the cancerous cells and the location in the large intestine.
Signs and symptoms:
- A feeling that your bowel doesn’t clear out entirely
- A persistent change in bowel habits, including diarrhea or constipation or a difference in the consistency of the stool
- Persistent abdominal discomforts, including cramps, gas or pain
- Rectal bleeding or blood in your stool
- Unexplained weight loss
- Weakness or fatigue
Treatment of Colon Cancer
Screening
Physicians recommend specific screening tests for healthy people with no signs or symptoms to look for signs of colon cancer or noncancerous colon polyps. Finding colon cancer at its earliest stage provides the most excellent chance for a cure. Screening has proven to reduce the risk of dying of colon cancer.
Doctors, in general, advise that people with an average risk of colon cancer begin screening around age 50. The American Cancer Society recommends

age 45. Additionally, individuals with a heightened risk, for example, those with a family history of colon cancer or African-American heritage, should consider screening sooner.
Several screening options exist — each with its benefits and drawbacks. A patient should discuss the options with their doctor, and together they can decide which tests are appropriate. If a colonoscopy is used for screening, polyps can be easily removed during the procedure before they turn into cancer.
Diagnosing
If a patient’s signs and symptoms indicate that they could have colon cancer, the doctor may recommend one or more tests and procedures, including:
- Colonoscopy. A colonoscopy uses a long, flexible, and slender tube attached to a video camera and monitor to view the entire colon and rectum. If any suspicious areas are located, the physician can pass surgical tools through the tube to take biopsies (tissue samples) for analysis as well as remove polyps. For more information on colonoscopy, please see the article, All About Colonoscopy, on this website.
- Blood tests. A blood test cannot tell a patient if they have colon cancer. But the doctor may test the blood for clues regarding overall health, for example, kidney and liver function tests.
The doctor may additionally test the blood for a chemical occasionally produced by colon cancers (carcinoembryonic antigen, or CEA). Tracked over time, the level of CEA in the blood may assist the doctor in understanding the diagnosis and whether the cancer is responding favorably to treatment.
If a patient has been diagnosed with colon cancer, a doctor may recommend tests to determine the extent (stage) of cancer. Staging helps decide what treatments are most appropriate.
Staging tests may incorporate imaging procedures such as abdominal, pelvic, and chest CT scans. In most cases, the stage of cancer may not be 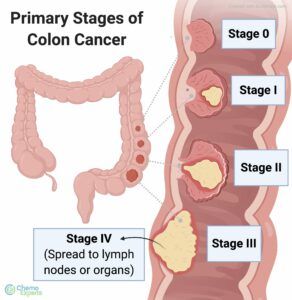 entirely resolved until after colon cancer surgery.
entirely resolved until after colon cancer surgery.
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV (4), with the lower stages representing cancer that is limited to the lining of the inside of the colon. By stage IV, the disease is deemed advanced and has spread (metastasized) to other areas of the body.
To summarize, if colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy, and drug treatments, such as chemotherapy, targeted therapy, and immunotherapy.
Prevention
Lifestyle changes
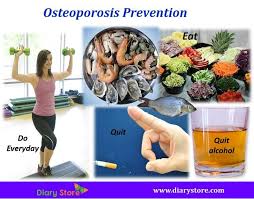
An individual can take steps to reduce the risk of colon cancer by making changes in his or her everyday life. It is advisable to:
- Diet. Eat a wide array of fruits, vegetables, and whole grains. Fruits, whole grains, and vegetables contain vitamins, minerals, fiber, and antioxidants, which could play a role in cancer prevention. It is wise to choose a variety of
 fruits and vegetables to enable one to get an array of vitamins and nutrients.
fruits and vegetables to enable one to get an array of vitamins and nutrients. - Alcohol. Drink alcohol in moderation, if at all. If an individual chooses to drink alcohol, he or she should limit the amount of alcohol they drink to no more than one (1) drink a day for women and two (2) for men.
- Quit smoking. If an individual smokes, they should talk to their doctor about ways to quit that may work for them.
- Exercise. An individual should exercise most days of the week by getting at least thirty (30) minutes of exercise on most days. But it is crucial to keep in mind that if you’ve been inactive, start slowly and build up gradually to 30 minutes. Also, consult with your physician before commencing any exercise program.
Maintain a healthy weight.
If you are at a healthy weight, work to maintain that weight by joining a healthy diet with regular, daily exercise. If you need to reduce weight, ask your doctor about healthy ways to achieve your goal. Endeavor to lose weight slowly by increasing the amount of exercise you perform and reducing the number of calories you eat.
Prevention for people with a high risk
Some medications are found to reduce the risk of precancerous polyps or colon cancer. For example, some evidence ties a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like drugs. But it is unclear what dose and what length of time would be required to reduce the risk of colon cancer. Additionally, taking aspirin on a daily basis has some risks, including gastrointestinal bleeding and ulcers.
These options are reserved for people with a high risk of colon cancer. There isn’t enough evidence to recommend these medications to individuals who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your heal care practitioner to determine whether preventive medications are safe for you.
Please feel free to leave any questions, comments, or concerns below.
Good Health!!
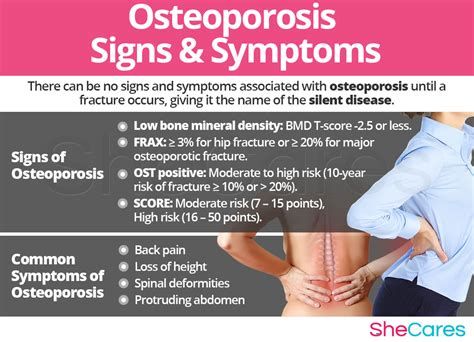
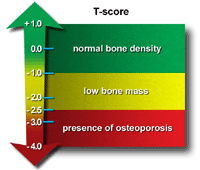 painless test, the patient lies on a padded table as a scanner passes over the body. In a majority of cases, only a few bones are checked — generally the hip and spine. A score of -2.0 or lower indicates an osteoporosis condition.
painless test, the patient lies on a padded table as a scanner passes over the body. In a majority of cases, only a few bones are checked — generally the hip and spine. A score of -2.0 or lower indicates an osteoporosis condition.
 and wrist. As such, maintaining appropriate body weight is good for bones just as it is for health in general.
and wrist. As such, maintaining appropriate body weight is good for bones just as it is for health in general.

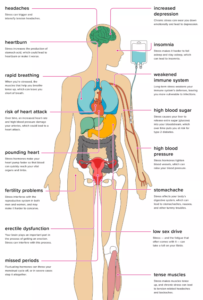 release the stress hormones adrenaline and cortisol. These hormones increase the heartbeat and send blood rushing to the areas where it is needed the most in an emergency, such as the muscles, heart, and other crucial organs.
release the stress hormones adrenaline and cortisol. These hormones increase the heartbeat and send blood rushing to the areas where it is needed the most in an emergency, such as the muscles, heart, and other crucial organs.