Mental illnesses are states of mind that affect mood, feeling, thinking, and behavior. They may be long-lasting (chronic), occasional, or they can affect the ability to relate to others and function on a daily basis. This article is going to cover one specific mental illness, depression. Depression is a widespread mental disorder that affects more than 264 million individuals of all ages worldwide. It is the leading cause of worldwide disability and a major purveyor to the burden of disease overall. Because of the enormity of depression, it is important to know about depression: the facts.
What is Depression?
Depression is a form of mental illness that is a mood disorder. It causes a perpetual feeling of sadness and loss of interest. Additionally called a major depressive disorder or clinical depression, it affects how one feels, thinks and, behaves, and can lead to a range of emotional and physical problems.
What Causes Depression?
Several factors can increase the chance of depression, including the following:
Substance abuse – Nearly 30% of individuals with substance abuse issues additionally have major or clinical depression. Even if drugs or alcohol temporarily makes one feel better, they will ultimately aggravate depression.
Death or a loss – Sadness or grief from the death or loss of a loved one, even if by natural means, can increase the risk of depression.
Abuse – Previous sexual, physical, or emotional abuse may increase the susceptibility to clinical depression later in life.
Certain medications – Certain drugs, for example, isotretinoin (used to treat acne), the antiviral drug interferon-alpha, and corticosteroids, can increase the risk of depression.
Conflict – Depression in an individual who has a biological susceptibility to develop depression may result from personal conflicts or disputes with friends or family members.
Genetics – A family history of depression can increase the risk. It is commonly thought that depression is a complex trait, which means that there are probably many different genes that each exerts minor effects, rather than a single gene that contributes to disease risk. The genetics of depression, as with most psychiatric disorders, are not as simple or straightforward as in solely genetic diseases such as Huntington’s chorea
or cystic fibrosis.
Key events – Even positive events such as starting a new job, graduating, or getting married may advance to depression. This can also include moving, losing a job or income, getting divorced, or retiring. Nevertheless, the syndrome of clinical depression is never just a “normal” response to stressful life events.
Serious illnesses – On occasion depression can co-exist with a major illness or may be triggered by another medical condition.
Additional personal problems – Problems such as social isolation because of other mental illnesses or being ostracized from a family or social group can contribute to the risk of developing clinical depression.
Types, Symptoms, and Treatment of Depression
Everybody feels down from time to time, but should an individual feels that way most of the time and it affects their daily life, chances are he or she may have clinical depression.
There are several different types of depression. Events in one’s life can cause some, and chemical changes in the brain can cause others. Therefore, it takes a specialist to determine which type of depression an individual may have and the best course of treatment.
Major Depression (major depressive disorder) – An individual who feels depressed most of the time for a majority, or all of the days of the week may have this type.
Some other symptoms might include:
- Being tired and without energy
- Feeling worthless or guilty
- Feeling on edge and disturbed, or else very lethargic and sluggish physically or mentally
- Lack of attention or pleasure in activities
- Thoughts of suicide
- Trouble concentrating or making decisions
- Problems going to sleep or feeling sleepy during the day
- Weight loss or gain
A physician may diagnose a patient with major depression if the individual has five (5) or more of these symptoms on most days for 2 weeks or longer. At least one among the symptoms must be a depressed mood or loss of interest in activities.
Treatment for major depression:
Meeting with a therapist can be of assistance. One can also meet with a mental health specialist who will assist in finding ways to manage the depression. Medications known as antidepressants can also be helpful.
When medication and therapy are not working, other options the physician may suggest are:
- Transcranial magnetic stimulation (TMS)
- Electroconvulsive therapy (ECT)
- Vagus Nerve Stimulation (VNS)
ECT makes use of electrical pulses, TMS uses a unique type of magnet, and VNS makes use of an implanted device. All are designed to accelerate particular areas of brain activity. This assists the parts of the brain that control one’s mood to work better.
Dysthymia (mild, chronic depression) – Dysthymia is less critical and doesn’t have as many symptoms as major depression. On the other hand, the symptoms can linger for a longer period of time, often two years or  longer. Individuals who suffer from dysthymia can additionally experience periods of major depression–sometimes known as double depression. In modern diagnostic classification systems, dysthymia and chronic depression are now both mentioned to as clinical depression disorder.
longer. Individuals who suffer from dysthymia can additionally experience periods of major depression–sometimes known as double depression. In modern diagnostic classification systems, dysthymia and chronic depression are now both mentioned to as clinical depression disorder.
The symptoms of dysthymia are the same as major depression but fewer in number and not as intense. They include the following:
- Being physically restless or rundown in a way that is noticeable by others
- Exhaustion or loss of energy almost daily
- Feelings of despair or insignificance or excessive guilt almost every day
- Insomnia or excessive sleep almost every day
- Loss of enjoyment in once pleasurable things
- A major change in weight (gain or loss of more than 5% of weight within a month) or appetite
- Difficulty with attentiveness or making decisions almost daily
- Frequent thinking of death or suicide, a suicide plan, or suicide attempt
- Sadness or down mood a majority of the day or almost daily
Treatment for Dysthymia
Although dysthymia is a serious illness, it is very treatable. As with any chronic illness, early detection and medical treatment may reduce the extent and duration of symptoms and in addition reduce the likelihood of developing an episode of major depression.
To treat dysthymia, physicians may use psychotherapy (talk therapy), medications such as antidepressants, or a mixture of these therapies. Frequently, dysthymia can be taken care of by a primary care physician.
Although Dysthymia is not as disabling as major depression, it can keep an individual from feeling their best and functioning optimally. Dysthymia can begin in childhood or adulthood and seems to be more common in women. According to the National Institute of Mental Health, roughly 1.5% of adult Americans are affected by dysthymia.
Atypical Depression – Atypical depression is a subtype. It can be an “identifier” for either major depression or dysthymic disorder. Individuals with atypical depression have usually experienced depression initially at an early age, during their teenage years.
Despite its name, atypical depression is extremely widespread. It is compared with “melancholic” depression, another subtype of depression that involves symptoms of insomnia (as opposed to oversleeping), loss of appetite (as opposed to increased appetite), a comparative lack of mood reactiveness to environmental circumstances, and a strikingly diminished ability to feel pleasure.
One of the main characteristics of atypical depression that differentiates it from melancholic depression is mood reactivity. In other words, the individual with atypical depression will see their mood improve if something positive occurs. On the other hand, with melancholic depression, positive changes will seldom yield a change in mood. Additionally, diagnostic standards call for at least two of the following symptoms to accompany the mood reactivity:
- Having a feeling of being weighed down, paralyzed, or “leaden”
- Having a more intense reaction or increased sensitivity to rejection, resulting in problems with social and work relationships
- Increased appetite or weight gain
- Sleeping too much (hypersomnia)
A physician will investigate physical causes for any of these symptoms. This would include a physical exam and diagnostic tests to look for a different issue such as hypothyroidism. With that condition, having low levels of thyroid hormone can lead to indicators that include depression and weight gain.
Treatment for atypical depression
Physicians are most likely to recommend psychotherapy (talk therapy) and/or medications for atypical depression, depending on the seriousness of the symptoms. There are various types of psychotherapy and medications available for treatment. An individual may be directed to a specialist such as a psychiatrist, psychologist, or other licensed mental health professional for treatment.
Postpartum Depression (PPD) – Postpartum depression (PPD) is a complicated combination of physical, emotional, and behavioral changes that happen in some females after giving birth to a child. According to the DSM-5, a manual used to diagnose mental disorders, PPD is a form of major depression that commences within 4 weeks after delivery. The diagnosis of postpartum depression is established not only on the length of time between delivery and commencement but also on the seriousness of the depression.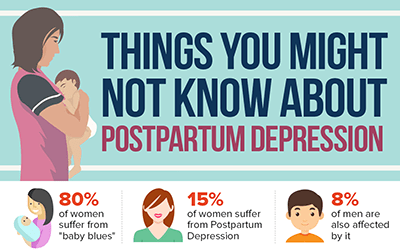
Postpartum depression is linked to chemical, social, and psychological changes that happen when having a baby. The term describes a range of physical and emotional changes that many new mothers experience. PPD can be treated with medication and counseling.
The chemical changes involve a rapid drop in hormones after delivery. The actual link between this drop and depression is not clear. However, what is known is that the amounts of estrogen and progesterone, the female reproductive hormones, intensify ten times over during pregnancy. Then, they drop severely after delivery. By three (3) days after giving birth, the levels of these hormones drop back to what they were before pregnancy.
In addition to these chemical changes, the social and psychological changes involved with having a baby create an increased risk of depression.
Most new mothers encounter the “baby blues” after delivery. Approximately 1 out of every 10 of these women will develop a more acute and longer-lasting depression post-delivery. About 1 in 1,000 women will develop a more severe condition called postpartum psychosis.
Symptoms of postpartum depression can be hard to detect. Because Scores of women have these symptoms following childbirth:
- Appetite changes
- Decreased libido
- Difficulty sleeping
- Excessive fatigue
- Frequent mood changes
With PPD, these are also accompanied by other symptoms of major depression, which are not typical after childbirth, and may include:
- Depressed mood
- Feelings of worthlessness, hopelessness, and helplessness
- Loss of pleasure
- Thoughts of death or suicide
- Thoughts of hurting someone else
New symptoms of obsessive-compulsive disorder (OCD) rarely occur during the postpartum period (about 1%-3% of women). When they do occur, the obsessions are generally related to concerns about the baby’s health or irrational fears of harming the baby. Panic disorder can also occur. A woman can have these conditions and depression at the same time.
Treatment for postpartum depression
Postpartum depression is treated differently depending on the type and intensity of a patient’s symptoms. Treatment options include anti-anxiety or antidepressant medications, psychotherapy, and involvement in a support group for emotional support and education. For extreme cases, intravenous infusion of a new medication called brexanolone (Zulresso) can be prescribed.
In the case of postpartum psychosis, drugs used to treat psychosis are usually added. Hospital admission is also frequently necessary.
If a woman is breastfeeding, medication can be a solution for depression, anxiety, or even psychosis. Under a doctor’s supervision, many women take medication while breastfeeding. This is a decision to be made between the patient and her doctor.
Untreated postpartum depression can be dangerous for new moms and their children. A new mom should seek professional help when:
- Feelings of extremely anxiousness, scared, and panicked most of the day
- Not able to cope with everyday situations
- Symptoms persist beyond 2 weeks
- Thoughts of harming herself or her baby
- Unable to function normally
Bipolar Disorder – Bipolar disorder, formerly called manic depression is a form of major affective disorder, or mood disorder, defined by manic or hypomanic episodes (changes from one’s normal mood accompanied by high-energy states).
Bipolar disorder is a grave condition. Mania often involves sleeplessness, sometimes for days, together with hallucinations, psychosis, grandiose 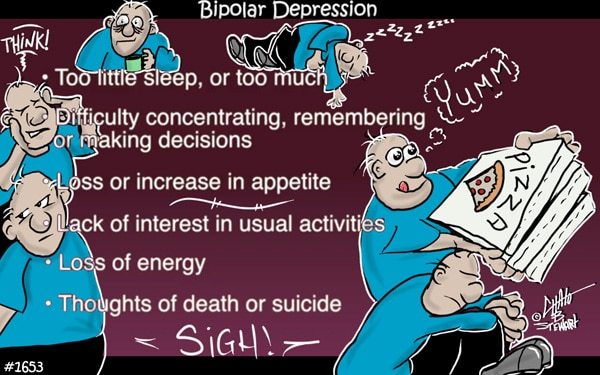 delusions, or paranoid rage. Also, depressive periods can be more harmful and harder to treat than in individuals who never have manias or hypomanias.
delusions, or paranoid rage. Also, depressive periods can be more harmful and harder to treat than in individuals who never have manias or hypomanias.
The seriousness of mood incidents can range from vastly mild to extreme, and they can happen slowly or suddenly within a period of days to weeks. When discrete mood incidents happen four (4) or more times per year, the succession is called rapid cycling. Rapid cycling should not be confused with very frequent moment-to-moment changes in mood, which can occasionally happen in individuals with bipolar disorder or other conditions such as borderline personality disorder.
Along with manic or depressive episodes, individuals with bipolar disorder may have disturbances in thinking. They may additionally have distortions of perception and impairment in social functioning.
The clinical depression symptoms seen with bipolar disorder are identical to those seen in major depressive disorder and include:
- Feelings of hopelessness, pessimism
- Difficulty concentrating, remembering, and making decisions
- Feelings of guilt, worthlessness, helplessness
- Insomnia, early-morning awakening, or oversleeping
- Lack of attention or enjoyment in hobbies and activities that were once enjoyed, including sex
- Fatigue, decreased energy, being “slowed down”
- Lasting physical symptoms that will not respond to treatment, like headaches, digestive disorders, and chronic pain
- Persistently sad, anxious, or “empty” moods
- Decreased desire for food and/or weight loss, or overeating and weight gain
- Restlessness, irritability
- Thoughts of death or suicide, suicide attempts
The signs of mania in bipolar disorder include:
- A reduced desire for sleep
due to high energy - Disconnected and very fast (racing) thoughts
- Grandiose beliefs
- Inappropriate elation or euphoria
- Inappropriate irritability
- Inappropriate social behavior
- Increased sexual desire
- Increased talking speed or volume
- Markedly increased energy
- Poor judgment and risk taking
Treatment for Bipolar Disorder
Treatment for bipolar disorder may involve the use of mood stabilizers such as lithium. Selected anticonvulsants, antipsychotics, and benzodiazepines may additionally be used to calm mood. Occasionally antidepressants are given in combination with mood stabilizers to give a boost to the depressed mood, although antidepressants are frequently not as effective as some mood stabilizers or specific atypical antipsychotics for treating depression in bipolar disorder.
Seasonal Depression (Seasonal Affective Disorder—SAD) – Seasonal depression is a mood disorder that occurs annually at the same time. An uncommon form of seasonal depression, known as summer depression, begins in late spring or early summer and ends in fall. In general, the seasonal affective disorder commences in fall or winter and terminates in spring or early summer.![Depression: the facts - Seasonal Affective Disorder [SAD]](https://universal-health-products.com/wp-content/uploads/2020/10/Depression-seasonal-2-776x1024.jpg)
While the specific triggers of SAD are not known, some scientists believe that certain hormones produced deep in the brain trigger attitude-related changes at certain times of the year. Experts believe that SAD may be linked to these hormonal changes. One (1) of several theories is that reduced sunlight during the fall and winter seasons leads to the brain generating less serotonin, a chemical linked to the brain pathways that control mood. When nerve cell pathways in the brain that regulate mood do not perform normally, the result can be feelings of depression, along with symptoms of fatigue and weight gain. For more information serotonin, please read the article, Serotonin: the facts on this website.
SAD usually begins in young adulthood and is more widespread in women than men. Some individuals with SAD have mild symptoms and feel out of sorts or irritable. On the other hand, others have worse symptoms that interfere with relationships and work.
Due to the fact that not enough daylight during wintertime is related to SAD, it’s less often found in countries where there’s plenty of sunshine year-round.
Individuals with SAD have many of the normal warning signs of depression that include:
Winter Symptoms
- Less energy
- Trouble concentrating
- Fatigue
- Greater appetite
- Increased desire to be alone
- Greater need for sleep
- Weight gain
Summer Symptoms
- Less appetite
- Trouble sleeping
- Weight loss
Treatment for SAD
There are diverse treatments, depending on the seriousness of symptoms. Also, if an individual has another type of depression or bipolar disorder, the treatment may be different.
Conventional antidepressants are frequently employed to treat seasonal depression. Bupropion XL is presently the only medication that is FDA-approved explicitly to prevent major depressive episodes in people with SAD.
Many physicians advise that people with SAD get outside early in the morning to get more light that is natural. If this is not possible for the reason of the dark winter months, antidepressant medications or light therapy (phototherapy) may help.
Psychotic Depression – Psychotic depression is another subtype of major depression that takes place when a severe depressive illness includes some form of psychosis (a condition that causes one to lose touch with reality).
The psychosis can be hallucinations (such as someone hearing a voice 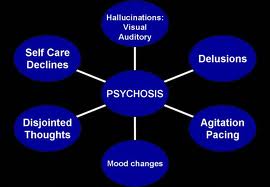 telling them that they are worthless and no good), delusions, or some other break with reality. They may also have strange and illogical ideas. Psychotic depression affects roughly one (1) out of every four (4) individuals admitted to the hospital for depression.
telling them that they are worthless and no good), delusions, or some other break with reality. They may also have strange and illogical ideas. Psychotic depression affects roughly one (1) out of every four (4) individuals admitted to the hospital for depression.
Usual symptoms for patients who have psychotic depression include:
- Agitation
- Anxiety
- Constipation
- Delusions or hallucinations
- Hypochondria
- Insomnia
- Intellectual impairment
- Physical immobility
Treatment for psychotic depression
Generally, treatment for psychotic depression occurs in a hospital setting. This allows the patient to have close monitoring by mental health professionals. Different meds are used to steady the person’s mood, usually including combinations of antidepressants and antipsychotic medications.
Antipsychotic drugs affect the neurotransmitters that permit communication between nerve cells in areas of the brain that control our ability to comprehend and manage information regarding the world around us. There are numerous antipsychotic, or neuroleptic, medications used regularly today. Each drug has distinctive side effects and may differ in its clinical efficiency profile. However, these drugs are better tolerated than the antipsychotics of the past.
Treatment for psychotic depression is very successful. Individuals are generally able to recover, usually within several months. However, continual medical follow-up may be needed. If the medications are unsuccessful in ending the psychosis and depression, occasionally electroconvulsive therapy (ECT) is used. It is crucial for the patient to work closely with the physician to find the most effectual drugs with the least amount of side effects, because psychotic depression is quite serious, and the risk of suicide is great also.
Treatment-Resistant Depression – Regrettably, depression treatments do not work always. As much as two-thirds of individuals with depression are not helped by the initial antidepressant they try. Up to a third, do not respond to many attempts at treatment.
Treatment-resistant depression (TRD) can leave one feeling despondent and disheartened. Months or even years can go by with no relief. In addition, after considering the effort it took to get help, it can be demoralizing with no sign of getting better.
However, there is hope. It is simply an issue of finding the right approach. This can include different drugs, therapy, and other treatments.
It is important to note that untreated clinical depression is a critical problem. Left untreated depression increases the chance of dangerous behaviors like drug or alcohol addiction. It can also ruin relationships, cause problems at one’s place of work, and make it challenging to overcome serious illnesses.
If you or someone you know is suffering from depression, you or they must get help as soon as possible.
Please feel free to leave any questions, comments, or concerns below.
Good Health!!
 chemicals. It powers brain processes and development, steroid hormone activity, and immune function.
chemicals. It powers brain processes and development, steroid hormone activity, and immune function.
 very reason.
very reason. relationship with folate, as they both depend on the other to function properly.
relationship with folate, as they both depend on the other to function properly.

 mouth.
mouth.